

- Avoidant/restrictive food intake disorder (ARFID) is an eating disorder not driven by body image or weight concerns.
- Instead, ARFID develops out of sensory sensitivities, a lack of appetite or food interest, or a fear that something bad will happen from eating.
- Equip is the largest ARFID treatment provider in the U.S. and has a proven track record of helping people recover gradually and safely from ARFID.

For a lot of us, food is a source of joy and pleasure. Many people even weave meals into rituals, whether on holidays or at everyday hangs with family or friends. But food isn’t fun for everyone.
Food can be a serious source of anxiety and distress if you have avoidant/restrictive food intake disorder (ARFID), formerly called “selective eating disorder.” ARFID isn’t like other eating disorders, even ones that also involve food restriction, like anorexia.
“ARFID is often misunderstood,” says Pam Skop, LMHC, CEDS, RPYT, an eating disorder specialist and the founder of EveryBody Psychotherapy NYC. “I explain it as an eating disorder not driven by body image or weight concerns, but by fear, sensory sensitivity, or distress related to food.”
She adds, “For some, that fear stems from a past choking incident or gastrointestinal pain. For others, it’s rooted in sensory overwhelm. Certain textures, smells, or temperatures can feel intolerable.”
In this article, we explore ARFID in adults, ARFID types, signs of ARFID, causes of ARFID, ARFID diagnosis, ARFID treatment, and more.
What is ARFID and how does it present in adults?
If you have, or suspect you have, ARFID, you’re not alone. The condition, which can seriously impact your health and quality of life, affects up to 15% of the general population. It affects both males and females, though some research indicates a slightly higher prevalence in people assigned male at birth—which sets it apart from other eating disorders, which are more commonly diagnosed in those assigned female.
ARFID doesn’t have as much awareness around it as other eating disorders, like anorexia. But awareness seems to be increasing—searches for info on ARFID have grown by 400% since 2022, according to Google Trends data. Additionally, health insurance claims for the diagnosis and treatment of ARFID increased by 305% from 2018 to 2022.
So what is ARFID? To understand ARFID, understanding what it is not is helpful. It’s not picky eating, which isn’t an eating disorder. When considering ARFID vs. picky eating, says Michelle Jones, PhD, a licensed clinical psychologist and clinical instructor at Equip. “A common misconception about ARFID is that individuals with ARFID are choosing to be picky or limit their intake out of stubbornness or oppositionality.”
But that’s not the case. “Many elements of how individuals with ARFID experience food are outside of their control and can have a significant impact on their social functioning, academic and work performance, and physical and mental health,” Dr. Jones adds.
People with ARFID may even have misconceptions about themselves, as well. “Adults with ARFID often describe their eating patterns as ‘picky’ or ‘childish,’” Skop says. “But that language hides the real issue, a nervous system stuck in a loop of avoidance and fear.”
ARFID is also vastly different from anorexia nervosa, an eating disorder with the most public awareness, for example. Characteristics of anorexia include a strong fear of gaining weight and using extreme efforts to prevent or counteract weight gain, such as severely restricting food, exercising to extremes, and more.
When considering ARFID vs. anorexia, people with ARFID restrict food intake, but they aren’t doing so because of a distorted body image or concerns about size, weight, or shape. Instead, people with ARFID avoid or restrict foods for other reasons, such as fear of discomfort after eating, aversions to food texture or taste, or a lack of interest in eating.
Understandably, these issues can be highly distressing and affect your overall health, happiness, and everyday life. Thankfully, working with a knowledgeable care team can help you cope with and recover from ARFID so that you feel more empowered regarding food and situations that involve eating.
The three types of ARFID
ARFID may present a little differently from person to person, but the symptoms fall into three categories or types. Each set of symptoms is associated with various mental health and neurodevelopmental comorbidities (other co-occurring conditions). But if you have ARFID, that doesn’t mean you have just one set of symptoms. “Each of these reasons represents a presentation of ARFID: sensory sensitivity, lack of interest, and fear of aversive consequences,” Dr. Jones says. “And people diagnosed with ARFID can experience one, two, or all three of these presentations.”

Sensory sensitivity/avoidant
People with this set of ARFID symptoms have food aversions based on sensory input. For example, textures, tastes, smells, colors, temperatures, or the appearance of some foods can cause disgust.
Common comorbidities include autism spectrum disorder (ASD) and sensory processing disorder (SPD). Although different, both these conditions can feature a hyperreactivity to sensory input.
Fear of aversive consequences
People with this set of ARFID symptoms experience food anxiety or fear of eating certain foods. They may fear consequences, such as choking, pain from eating or digesting food, or nausea or vomiting. In some cases, this type can arise from a food-related traumatic event, including a previous choking incident, allergen exposure, food poisoning that led to illness, and more.
Common comorbidities include anxiety disorders and obsessive compulsive disorder (OCD).
Lack of interest
People with this set of ARFID symptoms have a lack of interest in food. They may miss hunger cues, forget to eat, take little pleasure in eating, or have a low appetite in general.
A common comorbidity is attention deficit/hyperactivity disorder (ADHD), which impacts executive function, the mental skills you use to manage everyday tasks, problem-solve, and adapt to changes.
What causes ARFID in adults?
“While there’s no singular cause of ARFID and we are still learning about causes of ARFID,” Dr. Jones adds, “there are some biological and environmental factors that can contribute to ARFID developing.”
Genetics and biological factors
Genetics appear to play a significant role. A study looking at Swedish twins, ages 6 to 12, found that inherited factors accounted for 79% of the propensity toward the condition, while other factors (not shared between twins) accounted for about 21%. Other studies have linked appetite regulating hormone abnormalities to ARFID.
Genetic factors that might contribute include differences in taste processing and interoceptive awareness, which is your sensitivity to internal body sensations. For example, your body has mechanisms that tell your brain you’re hungry, but some people are more sensitive to those cues than others.
“There is some evidence of genetic influences of taste preferences and that having heightened sensitivity to sensory properties of food may run in families,” Dr. Jones says. “Individuals with sensory sensitivity and lack of interest often experience ARFID symptoms as early as the infant or toddler years and may find that their symptoms are exacerbated by childhood experiences.”
As an example, children whose preferences are routinely accommodated may be more likely to have difficulty trying and accepting new foods as they get older, she adds. Without intervention, ARFID symptoms that appear in early life tend to persist or worsen over time.
A traumatic event
ARFID may stem from a traumatic food-related event. Perhaps you endured a choking incident. Understandably, such a scary situation can lead to anxiety surrounding food and eating.
Or maybe you have food allergies and faced a severe allergic reaction to a specific food. Again, this experience may have caused intense fear, and you might worry about it happening again, especially in situations where you don't have access to a list of food ingredients. Avoiding an allergen, such as nuts, doesn’t mean you have ARFID, but you may be avoiding food in general out of fear of another allergic reaction. That behavior is consistent with ARFID.
“Individuals predisposed to anxiety may be more likely to experience ARFID symptoms following these types of events compared to those who are not predisposed to anxiety,” Dr. Jones says.
If these situations apply to you, that doesn’t mean you’re being picky or overly fearful. When a child undergoes a traumatic event or situation, researchers call it an adverse childhood experience (ACE). ACEs have links to disordered eating behaviors. An ACE could then lead to having ARFID as a child, or the eating disorder could manifest in adulthood. Likewise, any food-related traumatic experience in adulthood could lead to ARFID soon after or down the road.
Social and environmental factors
Trauma surrounding food isn’t limited to events such as choking or allergic reactions. Some social and environmental factors related to food can lead to a trauma response that then contributes to ARFID.
Food insecurity, such as not having enough money to buy food or having limited access to it, is an example. More than 85% of households in the United States experience some form of food insecurity. And it’s an issue that may have affected you as a child or as an adult, leading to ARFID at any age.
Other possibilities include having been shamed or mocked for eating or pressured to eat foods that you didn’t like. These issues in children may lead to the development of adult ARFID.
An underlying physiological condition
Many disorders affect the gastrointestinal (GI) tract, including irritable bowel syndrome (IBS), gastroesophageal disease (GERD), and inflammatory bowel disease (IBD), just to name a few.
With these conditions, certain foods, or even eating in general, can cause discomfort. Following a special diet as part of a treatment plan does not mean you have an eating disorder, but you may be avoiding food in general, again, out of fear of pain. If so, you might have ARFID.
The correlation doesn’t just apply to just GI issues. Conditions that feature chronic pelvic pain, such as endometriosis, also share associations with eating disorders.
Regardless of when you were diagnosed with a condition, whether in childhood or adulthood, the situation can lead to disordered eating. Many clinicians believe ARFID rates are higher in adult GI clinics compared to pediatric ones; one hypothesis is that ARFID develops after years of accumulated negative experiences with food or eating.
Psychological and developmental factors
As noted above with the different types of ARFID, this eating disorder sometimes coincides with other mental health or neurodevelopmental conditions, including generalized anxiety disorder (GAD), major depressive disorder (MDD), autism spectrum disorder (ASD), sensory processing disorder (SPD), obsessive compulsive disorder (OCD), and attention deficit/hyperactivity disorder (ADHD), as a few examples.
Symptoms of these conditions may contribute. For example, food texture aversion is associated with both ASD and SPD. And common concerns with ADHD include skipping meals or forgetting to eat. Both depression and anxiety can also lead to low appetite, general food disgust, or a specific texture aversion in adults or children.
Another way that these mental health and neurodevelopmental conditions may exacerbate ARFID symptoms is through medication side effects. Some medications, especially for ADHD, can cause a reduced appetite, which can worsen existing ARFID symptoms.
ARFID symptoms in adults
“The symptoms of ARFID can vary significantly depending on the presentation or presentations the individual is experiencing,” Dr. Jones says. Additionally, some ARFID symptoms typically show up in childhood rather than adulthood, or vice versa.
The following are some potential signs and symptoms of ARFID in adults:
- Anxiety about eating or food-related situations
- Anxiety about or refusing to try new or unfamiliar foods
- Avoidance of certain food textures, colors, smells, or temperatures
- Calorie restriction not motivated by body-image concerns
- Difficulty eating in social settings or with others watching
- Dizziness or faintness from poor nutrition
- Dry skin or brittle hair and nails from nutrient deficiencies
- Fatigue or low energy
- Fear of choking, vomiting, or gastrointestinal distress
- Food neophobia (reluctance or refusal to try new foods)
- Forgetting to eat
- Headaches related to undernutrition or dehydration
- Irritability or mood changes due to inadequate intake
- Low body weight (but not always a feature)
- Low interest in eating or appetite
- Malnutrition or micronutrient deficiencies
- Nausea when presented with non-“safe” foods
- Physical discomfort when eating feared or disliked foods
- Preoccupation with “safe” foods or meal rituals
- Refusal of entire food groups (e.g., fruits, vegetables, meats)
- Reliance on supplements or nutritional drinks instead of meals
- Restricted range of accepted foods (often fewer than 20 items)
- Rigidity about the types of foods eaten and how they are prepared
- Social withdrawal due to food-related embarrassment or anxiety
- Trouble concentrating or cognitive slowing from poor nutrition
- Weight loss or failure to maintain expected weight
If these symptoms seem familiar to you, you can assess whether you might have ARFID by taking this Equip screening quiz.
What ARFID looks like in adults vs. children
ARFID may present a little differently when comparing adults and children. Here are some key differences.
ARFID subtypes: children vs. adults and how they manifest
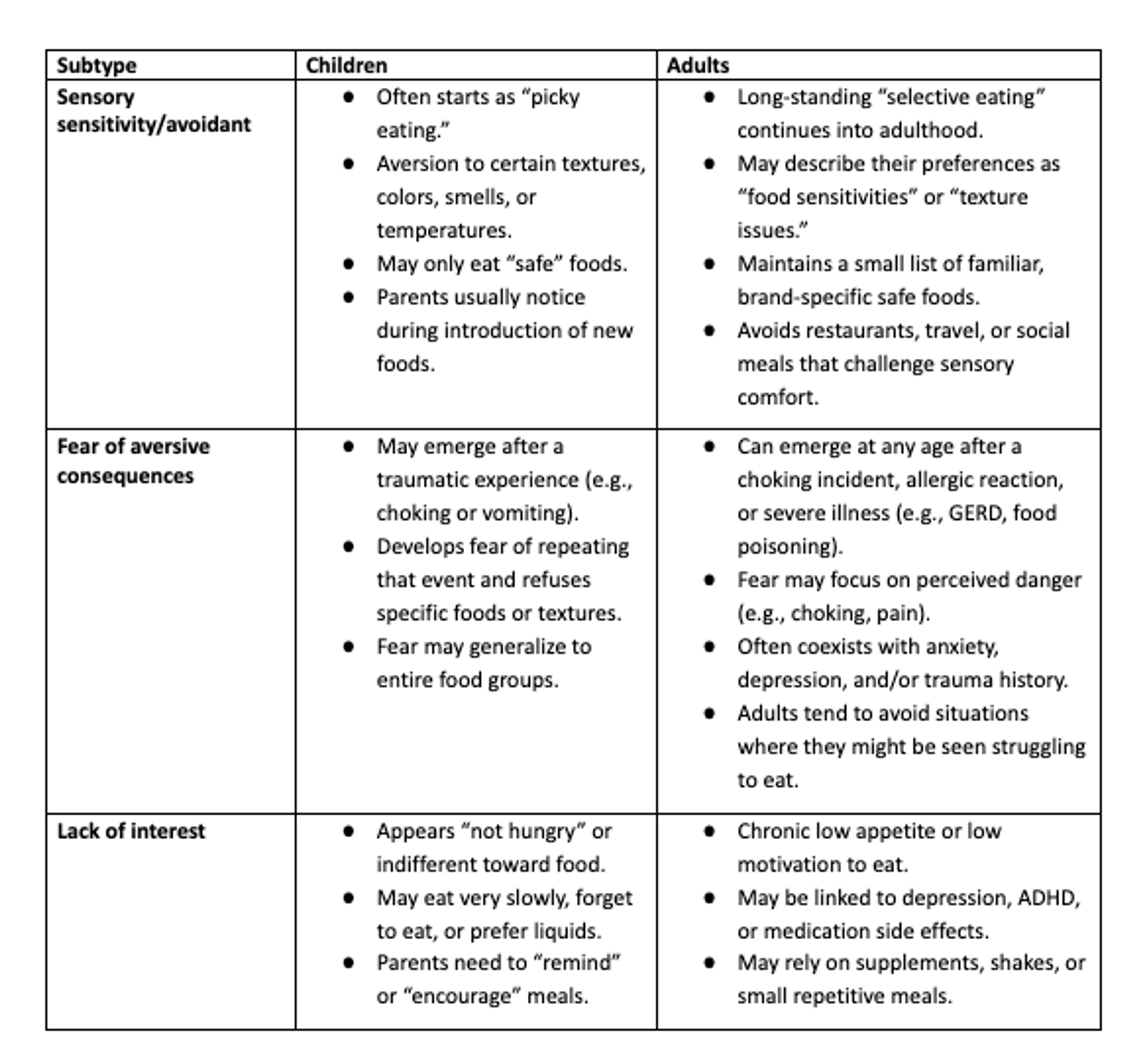

Dr. Jones expands on these differences with a few points: ARFID symptoms typically show up at an early age and can persist through someone’s whole life. Sensory sensitivities and lack of interest in food typically begin in infancy or early childhood—but may be more normalized at that time, too. “For example, a child with sensory sensitivity may have socially acceptable access to ‘kid-friendly’ foods that feel safe and may have less understanding of the negative impacts of a limited variety,” Dr. Jones explains. Fear of aversive consequences can develop at any point in time.
An adult, on the other hand, who only eats limited or specific foods “may not have access to preferred foods at social events and work functions,” Dr. Jones adds. This may lead to them limiting their social engagements “due to concern about judgment or may have greater insight into potential health consequences of a limited variety of food intake,” she adds.
Within each presentation of ARFID, symptoms are often similar regardless of age, but the impact of the symptoms can vary based on age.
How is ARFID diagnosed in adults?
Working with a clinician who has expertise in eating disorders, and specifically ARFID, is crucial. To diagnose ARFID, your clinician will ask you several questions or give you questionnaires or assessments.
The Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5) lists four criteria for an ARFID diagnosis:
- Criterion A: The following symptoms are present:
- Significant weight loss (or failure to maintain expected weight)
- Nutritional deficiency
- Dependence on supplements or tube feeding
- Marked interference with psychosocial functioning
- Criterion B: The disturbance is not due to lack of available food or culturally sanctioned practice, such as a fasting period or holiday.
- Criterion C: The disturbance does not occur exclusively during anorexia or bulimia nervosa, and a body-image disturbance isn’t present.
- Criterion D: The eating disturbance is not due to a medical condition. (Or if one is present, the severity of restriction exceeds what’s expected from that condition).
Your doctor will ask you questions regarding the following:
- Your medical history and your family’s
- Your history of mental health and neurodevelopmental conditions
- Your history of traumatic feeding experiences, if any
- Your history of GI conditions or abdominal and pelvic pain complaints
- Your symptoms and eating habits, including any changes and when they first began
Treatment for adults with ARFID
“Treatment often includes a multidisciplinary approach: therapy, nutritional support, and sometimes medical monitoring,” Skop says. “In therapy, we work to expand food flexibility through gradual exposure, nervous system regulation, and addressing underlying trauma or anxiety, rather than forcing compliance.”
Dr. Jones adds, “By utilizing a multidisciplinary team, the various ways in which ARFID can impact an individual’s social, emotional, and physical health can be fully addressed.”
One caveat: “It is important that the members of the care team have knowledge of and experience in treating ARFID to ensure that effective techniques are being implemented to adequately and appropriately address symptoms,” Dr. Jones says.
Keep in mind that treatment for children with ARFID differs from that of adults. For children, treatment involves working with parents or guardian caregivers alongside the child. For adults, the focus is on empowering you.
Here are a few treatment possibilities for adults:
Cognitive behavioral therapy for ARFID (CBT-AR)
CBT in general focuses on identifying and challenging negative thought patterns and behaviors with the intent of developing healthier coping mechanisms. CBT-AR focuses on thoughts, feelings, and behaviors surrounding food and eating.
You’ll work closely with a therapist to learn more about ARFID and how it manifests. CBT-AR also typically involves self-monitoring between sessions, to help increase awareness of your eating behaviors and make changes. CBT-AR also includes different treatment approaches specifically designed to address the three different drivers of ARFID—so the treatment can be personalized to address your unique set of symptoms.
At Equip, your therapist will administer CBT-AR, but you also have access to a medical provider and dietitian to help with weight restoration and a peer mentor who can provide support based on lived experience.
Exposure and response prevention (ERP)
This type of therapy is often a component of CBT-AR. It focuses on gradual exposure to foods and settings related to eating.
This treatment is usually used to address ARFID symptoms associated with a specific fear of eating. You and your therapist will identify a list of foods and situations that trigger your fears and create a hierarchy of these situations. Then, you and your therapist will work on gradual exposure to these things, starting with the least distressing first and building exposure from there. The goal is to help you learn that these foods and situations are actually safe or that you can tolerate distress.
A key focus of ERP is the response prevention component. Your therapist will guide you on how to resist your usual avoidance behavior, such as seeking reassurance or checking labels. As you progress, you learn healthier coping mechanisms to deal with anxiety or distress surrounding meals. And you can even continue the process on your own after initial treatment.
Virtual care for ARFID
Virtual care can be particularly valuable for those dealing with ARFID. It’s on par with in-person care, and it offers unique benefits such as convenience. For busy adults juggling the demands of work and families, virtual care, through a service such as Equip Health, can accommodate already-packed schedules and eliminate the need to commute.
Peer support
In addition to one-on-one therapy, you may also find support groups with other people who have ARFID helpful. Equip features a host of options.
Medications
The Food and Drug Administration (FDA) has not approved any medications to specifically treat ARFID. However, your provider might prescribe medications to treat underlying issues that are contributing to the disorder, such as anxiety, depression, and more. In some cases, they may prescribe a medication off label (meaning for a use other than originally intended). There are a number of medications, such as Periactin or cyproheptadine, that have been used to help increase appetite.
When to seek help
“People should seek help when avoidance begins to interfere with health, social connection, or emotional well-being,” Skop says. “Healing isn’t about eating ‘normally.’ It’s about rebuilding safety and trust in the body’s relationship with food.”
“If someone suspects that they or their loved one has ARFID symptoms,” Dr. Jones says, “it is important to seek evaluation from a professional who is experienced in diagnosing eating disorders, including ARFID.”
“At Equip, all providers are trained in evidence-based approaches for treating ARFID and use these approaches to target the specific symptom set each individual identifies during the intake process,” she says. “We utilize a patient-centered approach, backed by research to support patients in achieving their physical, nutritional, and psychosocial goals.”
You should seek urgent help if you are experiencing any of the following related to ARFID:
- Abnormal heart rate, such slow, fast, or irregular
- Dizziness or fainting
- Dehydration
- Dependence on supplements or liquid nutrition options
- Frequent illness due to poor nutrition
- Low body weight
- Low blood pressure
- Low body temperature
- Nutritional deficiencies
- Seizures
- Suicidal thoughts
The bottom line
ARFID recovery will be different for everyone. Although recovery may not lead you to crave all foods or to love all situations related to eating, it can help you expand your options, ease anxiety about food, and improve your nutrition, overall health, and well-being. Most importantly, anyone who is dealing with ARFID or another ED should know that recovery is possible at any age, regardless of how long you've been struggling. Recovery is not always straightforward, and it can be difficult, but it’s worth the effort to achieve the healthy and fulfilling life you deserve.
FAQ
How do you treat ARFID in adults?
In adults, avoidant/restrictive food intake disorder (ARFID) requires a multidisciplinary approach that may include cognitive behavioral therapy for ARFID (CBT-AR), a method for recognizing and challenging negative thoughts, feelings, and behaviors surrounding specific foods and eating and working to develop better coping mechanisms. A component of CBT-AR is exposure and response prevention (ERP), which is a step-based approach to expanding your food options and more. Group support and medications may also help with your recovery.
What are the three types of ARFID?
The three types of avoidant/restrictive food intake disorder (ARFID) include sensory sensitivity/avoidant, fear of aversive consequences, and lack of interest. People with the sensory sensitivity/avoidant type have food aversions based on sensory input, such as texture or taste. People with the fear of aversive consequences type may fear choking, pain from eating or digesting food, or nausea or vomiting. People with the lack of interest type may miss hunger cues, forget to eat, or have a low appetite in general.
Is ARFID a mental illness?
Yes, avoidant/restrictive food intake disorder (ARFID) is an eating disorder, and eating disorders are considered mental illnesses.
Can you develop ARFID as an adult?
Yes, you can develop avoidant/restrictive food intake disorder (ARFID) as an adult. Many factors may play a role, including traumatic experiences related to food, genetics, underlying mental health or neurodevelopmental disorders, and more.
“ARFID | Symptoms, Treatment, & Support | NEDA.” National Eating Disorders Association, https://www.nationaleatingdisorders.org/avoidant-restrictive-food-intake-disorder-arfid/. Accessed 15 Nov. 2025.
Aupetit, Alexandra, et al. “Association between Endometriosis, Irritable Bowel Syndrome and Eating Disorders: ENDONUT Pilot Study.” Journal of Clinical Medicine, vol. 11, no. 19, Sept. 2022, p. 5773. pmc.ncbi.nlm.nih.gov, https://doi.org/10.3390/jcm11195773.
Becker, Kendra R., et al. “Ghrelin and PYY in Low-Weight Females with Avoidant/Restrictive Food Intake Disorder Compared to Anorexia Nervosa and Healthy Controls.” Psychoneuroendocrinology, vol. 129, Apr. 2021, p. 105243. pmc.ncbi.nlm.nih.gov, https://doi.org/10.1016/j.psyneuen.2021.105243.
Białek-Dratwa, Agnieszka, et al. “Neophobia—A Natural Developmental Stage or Feeding Difficulties for Children?” Nutrients, vol. 14, no. 7, Apr. 2022, p. 1521. pmc.ncbi.nlm.nih.gov, https://doi.org/10.3390/nu14071521.
Brigham, Kathryn S., et al. “Evaluation and Treatment of Avoidant/Restrictive Food Intake Disorder (ARFID) in Adolescents.” Current Pediatrics Reports, vol. 6, no. 2, Apr. 2018, p. 107. pmc.ncbi.nlm.nih.gov, https://doi.org/10.1007/s40124-018-0162-y.
Chen, Na, et al. “Relationships between Autistic Traits, Taste Preference, Taste Perception, and Eating Behaviour.” European Eating Disorders Review, vol. 30, no. 5, June 2022, p. 628. pmc.ncbi.nlm.nih.gov, https://doi.org/10.1002/erv.2931.
D’Adamo, Laura, et al. “Prevalence, Characteristics, and Correlates of Probable Avoidant/Restrictive Food Intake Disorder among Adult Respondents to the National Eating Disorders Association Online Screen: A Cross-Sectional Study.” Journal of Eating Disorders, vol. 11, no. 1, Dec. 2023, p. 214. DOI.org (Crossref), https://doi.org/10.1186/s40337-023-00939-0.
Finn, Daphna M., et al. “Pharmacotherapy for Attention Deficit/Hyperactivity Disorder in Youth with Avoidant Restrictive Food Intake Disorder: A Case Series of Patients Prescribed Stimulant Medication in a Partial Hospitalization Program for Eating Disorders.” Journal of Eating Disorders, vol. 11, Dec. 2023, p. 226. pmc.ncbi.nlm.nih.gov, https://doi.org/10.1186/s40337-023-00954-1.
Food Security in the U.S. - Key Statistics & Graphics | Economic Research Service. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/key-statistics-graphics. Accessed 15 Nov. 2025.
From 2018 to 2022, Eating Disorder Claim Lines Increased 65 Percent Nationally as a Percentage of All Medical Claim Lines. http://www.fairhealth.org/article/from-2018-to-2022-eating-disorder-claim-lines-increased-65-percent-nationally-as-a-percentage-of-all-medical-claim-lines. Accessed 15 Nov. 2025.
Ghaffari, Affan, et al. “Associations of Adverse Childhood Events with Disordered Eating Behaviors among US Adolescents.” Eating Behaviors, vol. 55, Dec. 2024, p. 101929. ScienceDirect, https://doi.org/10.1016/j.eatbeh.2024.101929.
Kaşak, Meryem, et al. “Selective Eating and Sensory Sensitivity in Children With ADHD: A Comparative Study of ARFID Symptom Profiles.” The International Journal of Eating Disorders, vol. 58, no. 10, Oct. 2025, pp. 1991–2002. PubMed, https://doi.org/10.1002/eat.24512.
Keski-Rahkonen, Anna, and Anu Ruusunen. “Avoidant-Restrictive Food Intake Disorder and Autism: Epidemiology, Etiology, Complications, Treatment, and Outcome.” Current Opinion in Psychiatry, vol. 36, no. 6, Nov. 2023, pp. 438–42. PubMed, https://doi.org/10.1097/YCO.0000000000000896.
Khalsa, Sahib S., et al. “Interoception and Mental Health: A Roadmap.” Biological Psychiatry. Cognitive Neuroscience and Neuroimaging, vol. 3, no. 6, Dec. 2017, p. 501. pmc.ncbi.nlm.nih.gov, https://doi.org/10.1016/j.bpsc.2017.12.004.
Laboe, Agatha A., et al. “The Relation of Food Insecurity to Eating Disorder Characteristics and Treatment-Seeking among Adult Respondents to the National Eating Disorders Association Online Screen.” Eating Behaviors, vol. 50, June 2023, p. 101776. pmc.ncbi.nlm.nih.gov, https://doi.org/10.1016/j.eatbeh.2023.101776.
Menzel, Jessie E., and Taylor R. Perry. “Avoidant/Restrictive Food Intake Disorder: Review and Recent Advances.” Focus: Journal of Life Long Learning in Psychiatry, vol. 22, no. 3, June 2024, p. 288. pmc.ncbi.nlm.nih.gov, https://doi.org/10.1176/appi.focus.20240008.
Moore, Christine A., and Brooke R. Bokor. “Anorexia Nervosa.” StatPearls, StatPearls Publishing, 2025. PubMed, http://www.ncbi.nlm.nih.gov/books/NBK459148/.
Ptacek, Radek, et al. “Disruptive Patterns of Eating Behaviors and Associated Lifestyles in Males with ADHD.” Medical Science Monitor : International Medical Journal of Experimental and Clinical Research, vol. 20, Apr. 2014, p. 608. pmc.ncbi.nlm.nih.gov, https://doi.org/10.12659/MSM.890495.
Ramirez, Zerimar, and Sasidhar Gunturu. “Avoidant Restrictive Food Intake Disorder.” StatPearls, StatPearls Publishing, 2025. PubMed, http://www.ncbi.nlm.nih.gov/books/NBK603710/.
Thomas, Jennifer J., et al. “Avoidant/Restrictive Food Intake Disorder: A Three-Dimensional Model of Neurobiology with Implications for Etiology and Treatment.” Current Psychiatry Reports, vol. 19, no. 8, Aug. 2017, p. 54. pmc.ncbi.nlm.nih.gov, https://doi.org/10.1007/s11920-017-0795-5.
Velimirović, Mina, et al. “Anxiety, Obsessive‐Compulsive, and Depressive Symptom Presentation and Change Throughout Routine Eating Disorder Treatment.” European Eating Disorders Review, vol. 33, no. 3, May 2025, pp. 490–502. DOI.org (Crossref), https://doi.org/10.1002/erv.3160.







