

The information in this article originally appeared in an Equip Academy presentation. Watch the presentation here, and register for future Equip Academy events to learn about other eating disorder-related topics and earn free CE credits.
Screening for eating disorders is essential to ensuring that patients don’t slip through the cracks and that everyone who is struggling gets the support they need. However, many providers aren’t equipped with the knowledge and tools required to properly screen for these illnesses. Today, I’ll explain everything providers should know about screening for eating disorders.
What is screening?
First, let’s define what screening is and why it’s important. At their broadest definition, screenings are medical tests used to check for diseases and health conditions before there are any signs or symptoms. According to the World Health Organization, “the purpose of screening is to identify people in an apparently healthy population who are at higher risk of a health problem or a condition, so that an early treatment or intervention can be offered and thereby reduce the hospitalization, incidence, and/or mortality of the health problem or condition within the population.”
Some examples of screening options include:
- A routine survey at each checkup
- Questions from a clinician during exams
- Routine testing of blood, vitals, imaging, etc.
Screening is essential for eating disorders for a few reasons. First, the lag between the onset of eating disorder symptoms and treatment is on average five to seven years. We know that early detection and swift entry into treatment can improve outcomes, and so this lag is significant.
And secondly, misconceptions and stereotypes about eating disorders mean that many people with these illnesses go undiagnosed—just 20 to 25% of patients with an eating disorder actually get treatment, and this number is even smaller for marginalized groups. Eating disorders are still thought of as a niche issue, despite prevalence similar to other mental health disorders, and newer diagnoses like ARFID and OSFED are identified less often. More screening would shed light on the millions of people with eating disorders and make clear that more accessible treatment is needed.
Screening options
There are a number of different options for screening for eating disorders in patients. Below, we’ll go through some of the screening tools used for different patient populations.
Screeners for adults
SCOFF
The SCOFF questionnaire is a series of five questions. An answer of “yes” to
two or more questions indicates the need for a more comprehensive assessment.
Questions:
S: Do you make yourself Sick because you feel uncomfortably full?
C: Do you worry you have lost Control over how much you eat?
O: Have you recently lost more than One stone (6.35 kg) in a three-month period?
F: Do you believe yourself to be Fat when others say you are too thin?
F: Would you say Food dominates your life?
The SCOFF’s strengths are that there is lots of research on it; it is accurate at distinguishing those with an eating disorder from those without an eating disorder; it’s brief and easy to score; and there’s a low likelihood of false alarms.
Its limitations are that it is primarily focused on anorexia and bulimia, so is less accurate for diagnosing binge eating disorder (BED), other specified feeding or eating disorder (OSFED), or avoidant/restrictive food intake disorder (ARFID); it only raises a red flag after symptoms have started; it is only validated in adults; it is less accurate in studies that include men; and it does not pick up on disordered exercise behaviors.
Eating Disorder Screen for Primary Care (ESP)
In this screener, responses are classified as normal or abnormal. A “no” to question one is classified as an abnormal response, and a “yes” to questions two through five is classified as an abnormal response. Any abnormal response indicates that the patient needs further assessment. Research shows that the best individual questions for ruling out an eating disorder are questions one and three.
Questions:
1. Are you satisfied with your eating patterns?
2. Do you ever eat in secret?
3. Does your weight affect the way you feel about yourself?
4. Have any members of your family suffered with an eating disorder?
5. Do you currently suffer with, or have you ever suffered in the past, with an eating disorder?
The strengths of the ESP are that it is conversational, short, has simple scoring, and there is a high likelihood of not missing any cases. Its limitations include the fact that it is only used in one study and a few case studies, so there is less validation, and it is prone to more false positives.
Screener for Disordered Eating (SDE)
In this screener, each item is scored one if present, and a score of two or more is predictive of the presence of an eating disorder.
Questions:
1. Do you often feel the desire to eat when you are emotionally upset or distressed?
2. Do you often feel you cannot control what or how much you eat?
3. Do you sometimes make yourself throw up (vomit) to control your weight?
4. Are you often preoccupied with the desire to be thinner?
5. Do you believe yourself to be fat when others say you are thin?
The strengths of the SDE screener are that it is brief, and similar to SCOFF but with questions that improve accuracy for BED. Its limitations include the fact that there are still no questions that would catch ARFID; it is only used in adults; and it only picks up after more severe symptoms have started.
Eating Disorder Examination Questionnaire-7 (EDEQ-7)
This screener is based on the full EDEQ, but pared down to focus on dietary restraint, shape and weight valuation, and body satisfaction.
Questions:
1. Have you been consciously trying to limit the amount of food you eat to influence your shape or weight?
2. Have you attempted to avoid eating any foods which you like in order to influence your shape or weight?
3. Have you attempted to follow definite rules regarding your eating in order to influence your shape or weight; for example, a calorie limit, a set amount of food, or rules about what or when you should eat?
4. Has your weight influenced how you think about (judge) yourself as a person?
5. Has your shape influenced how you think about (judge) yourself as a person?
6. How dissatisfied have you felt about your weight?
7. How dissatisfied have you felt about your shape?
The strengths of the EDEQ-7 are that it is briefer than the full EDE-Q, but still maintains the quality and validation of the full questionnaire. Its limitations are that it is lower in accuracy than the full EDE-Q, so may miss some cases; it also does not include questions about ARFID.
Screeners for college-age youth
Stanford-Washington University Eating Disorder Screen (SWED)
The SWED is primarily for college-age women. It is embedded into the screener on NEDA’s website.
Its strengths are that it is comprehensive; has lots of good validation; and is tested most widely across diagnoses. Its limitations are that it is only applicable to a subset of those with eating disorders; accuracy is lower for OSFED; has very little data in men and racial or ethnic minority groups; and is lengthy and somewhat complex to score.
The NEDA screener has a wide reach, with 71,362 people taking the screener. Of that group, 86.3% screened positive for a possible clinical or subclinical eating disorder—but only 14% report receiving treatment.
Brief Assessment of Stress and Eating (BASE)
The BASE screener is based on the full Eating Pathology Symptoms Inventory (EPSI), but is pared down to focus on specific behaviors and cognitions. It is for student healthcare and college research settings.
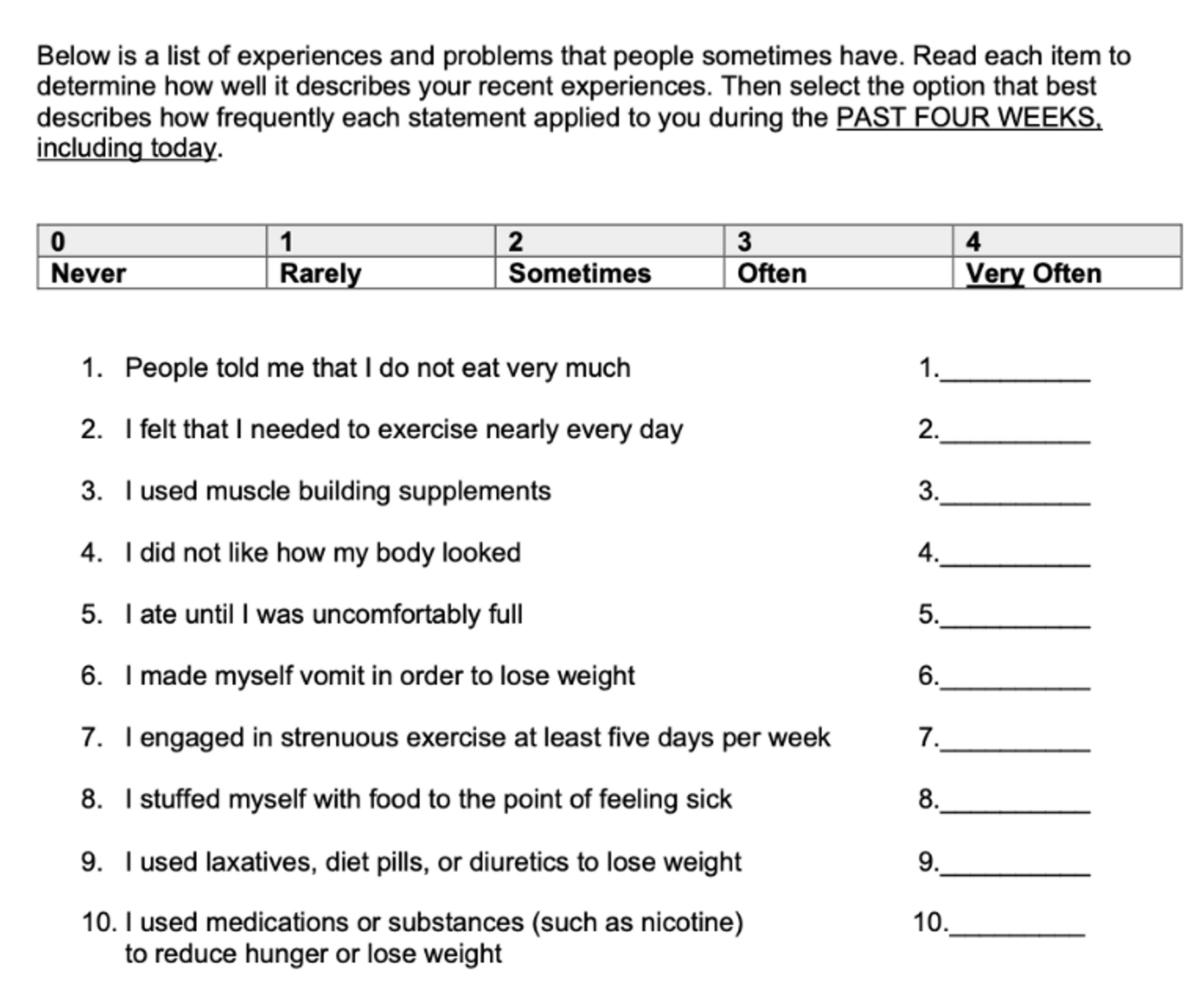
Its strengths are that it is brief, captures a more diverse range of behaviors, and has strong outcomes in men and gender diverse populations. Its main limitation is that it only applies to a select population of young adults.
ARFID screeners
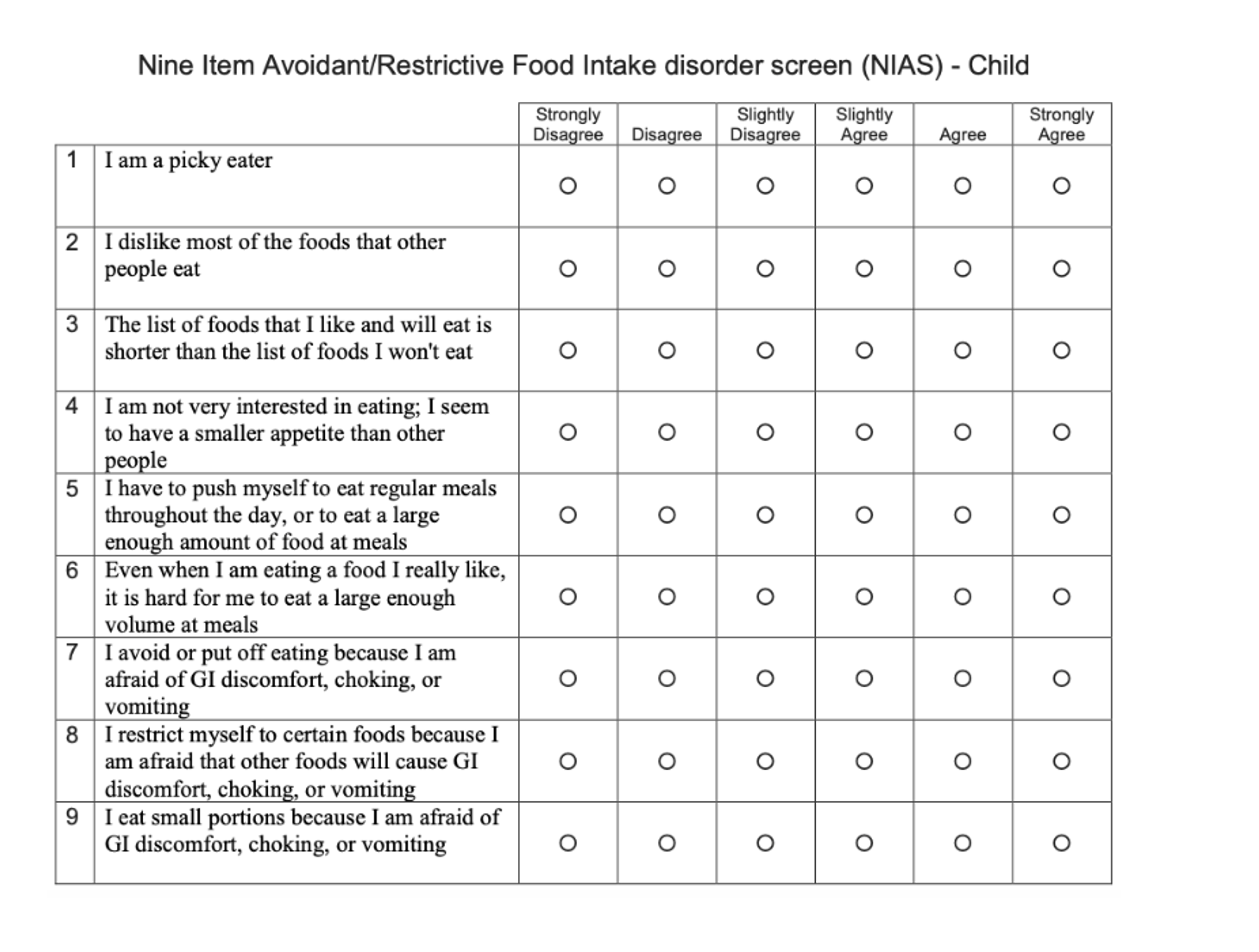
Nine Item ARFID Screen (NIAS)
This screener distinguishes between ARFID subtypes: selective eating, lack of interest/low appetite, and fear of aversive consequences. Scores of >9 or 10 indicate a potential diagnosis.
Its strengths are that it is brief, provides clarity on presentation types, is validated in youth and gender diverse groups, and is translated into multiple languages. Its main limitation is that it doesn’t rule out other eating disorders.
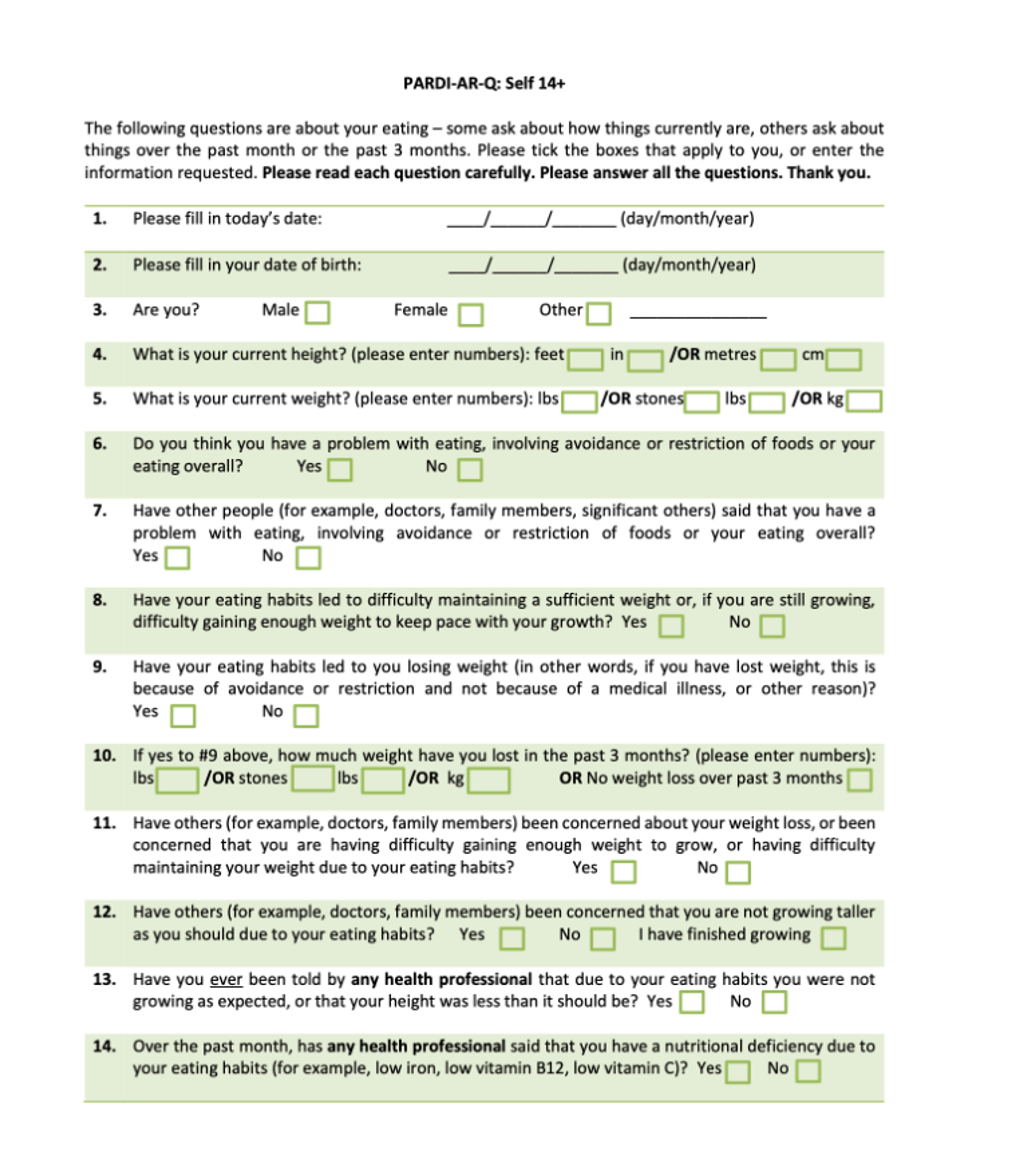
Pica, ARFID, Rumination Disorder Interview - ARFID - Questionnaire (PARDI-AR-Q)
The PARDI-AR-Q is a 32-item questionnaire based on the diagnostic interview. Its strengths are that it can provide information on ARFID subtypes, has a screening algorithm, is comprehensive, and there’s a patient version as well as a parent version for kids as young as age four. Its limitations are that it’s a longer survey, has complicated scoring, and there are no validation studies yet for screening.
Below is a sampling of the questionnaire.
Use of screeners in clinical practice
So how can providers incorporate these screeners into clinical practice? There are few important things to keep in mind when it comes to using the screeners outlined above. Some tips and tools to remember:
- Incorporate screening tools early
- Integrate behavioral health screeners into existing medical screeners, like growth charts
- Recognize that screening doesn’t mean diagnosis, and further assessment is always needed
- Have referral sources handy
The SBIRT model is also an important concept to understand. SBIRT stands for Screen, Brief Intervention, and Referral to Treatment. If the screening is positive, the healthcare professional asks further questions to assess level of use. For high-risk use, a brief intervention is recommended; for severe use, a referral to treatment is recommended. The SBIRT approach has been shown to be valid for identifying and improving outcomes for people who have high risk use of alcohol and drugs.
The SBIRT-ED is a novel screening tool for adults in primary care. After screening, the tool walks you through a brief intervention and resources for referral.
Gaps, limitations, and what’s next
We need more research on eating disorder screening. There are currently no validated screeners for youth, and evidence for adult and adolescent screening (among asymptomatic patients) has been deemed insufficient, despite the many screeners that are available. The current state of eating disorder screening is considered insufficient for a few reasons:
- There are no studies directly assessing the benefits and harms of screening, which is needed
- They are mostly assessed in adult women, and available data lack information about underrepresented groups
- Treatment trials did not recruit screen-detected participants from primary care settings
- Limited generalizability to populations who would be detected by routine screening
In addition to refining and further researching screening tools, it’s also important that screening begin earlier. Eating disorders often peak in childhood or adolescence, making youth a high-risk time for onset—yet there are no screeners developed for kids 12 and under. There are limited validated screening tools for adolescents, but many of the adult ones are used with teens. A tool for youth needs to focus on catching early symptoms of an eating disorder, and be relevant to the symptoms we expect to show up in this age group (e.g., ARFID). It’s likely that parents or other caregivers may be the best source for administering these screeners.
There are currently a number of in-progress studies looking to create clinically-validated screeners for youth. These include studies from Equip, AED/AAP Workgroup, and The CARE Lab at the University of Kansas.
For more information on screening for eating disorders, as well as in-depth information about the Equip research team’s pediatric ED screener, watch my recorded Equip Academy presentation on the topic. You can also explore past Equip Academy presentations and register for upcoming events here.
- Screening programmes: a short guide. Increase effectiveness, maximize benefits and minimize harm. Copenhagen: WHO Regional Office for Europe; 2020.
- Hamilton A, et al. Understanding treatment delay: Perceived barriers preventing treatment-seeking for eating disorders. Aust N Z J Psychiatry. 2022 Mar;56(3):248-259. doi: 10.1177/00048674211020102
- Penwell TE, et al.. Eating Disorder Treatment Access in the United States: Perceived Inequities Among Treatment Seekers. Psychiatric Services [Internet]. https://psychiatryonline.org/doi/full/101176/appi.ps.20230193. American Psychiatric Publishing; 2024 May 8 [cited 2024 Jul 14];0(0).
- Graham AK, et al., A screening tool for detecting eating disorder risk and diagnostic symptoms among college-age women. J Am Coll Health. 2019 May-Jun;67(4):357-366. https://www.nationaleatingdisorders.org/screening-tool/







