

- Other specified feeding or eating disorder (OSFED) is an umbrella term used for diagnosing an eating disorder that doesn’t meet the full criteria for a separate diagnosis.
- OSFED is just as serious as other more well-known eating disorders and can increase the risk of severe physical and mental health concerns.
- Treatment is available and recovery is possible with the help of a knowledgeable care team.

When I was in my teens and early 20s, I knew my behaviors surrounding food and exercise were somehow disordered. But I didn’t have a name for my concerns. Instead, I felt as if my brain had cherry-picked behaviors or criteria from several different eating disorders and created a version all its own.
Not having a term for what I was going through was frustrating. I knew I needed help, but without a clear definition for my behaviors and thought patterns, I didn’t think I was “sick enough” to ask for that care. I delayed seeking treatment until a friend finally recommended an appropriate therapist and encouraged me to make an appointment.
Eventually, that wonderful clinician gave me a name for what was going on. She called it eating disorder not otherwise specified (EDNOS). Nowadays the language has shifted, and EDNOS is referred to as otherwise specified feeding or eating disorder (OSFED).
If you or a loved one is experiencing disordered eating or exercise behaviors that don’t fit under a certain label, you might be searching for answers about what’s going on so that you can get the right care. Know that no matter what you’re noticing, treatment is available, and recovery is possible.
In this article, we explore OSFED diagnostic criteria, OSFED symptoms, OSFED treatment, OSFED vs. EDNOS, and more.
What is other specified feeding and eating disorder (OSFED)?
“In simple terms,” says, Rachel Levine, LMFT, LSWA, CEAP, a therapist at Equip,“it means someone is struggling with serious and disordered eating-related thoughts or behaviors that don’t fit neatly into one specific diagnosis, like anorexia or bulimia, but are just as real and have just as strong an impact in their life. It’s not a ‘lesser’ eating disorder; it’s a way clinicians name patterns that fall outside strict boxes.”
OSFED diagnostic criteria:
- You or a loved one presents with clinically significant symptoms of an eating or feeding disorder.
- The symptoms cause distress or impaired functioning.
- The presentation does not meet the full diagnostic criteria for another feeding or eating disorder.
Levine makes an important point: OSFED, or EDNOS, as it used to be called, is not a less-severe eating disorder compared to others. But that can be a common misconception, and it was for me. My behaviors and symptoms didn’t fully align with anorexia nervosa or bulimia nervosa, for example, so I didn’t seek help. Yet what I was doing was still dramatically impacting my physical and mental health.
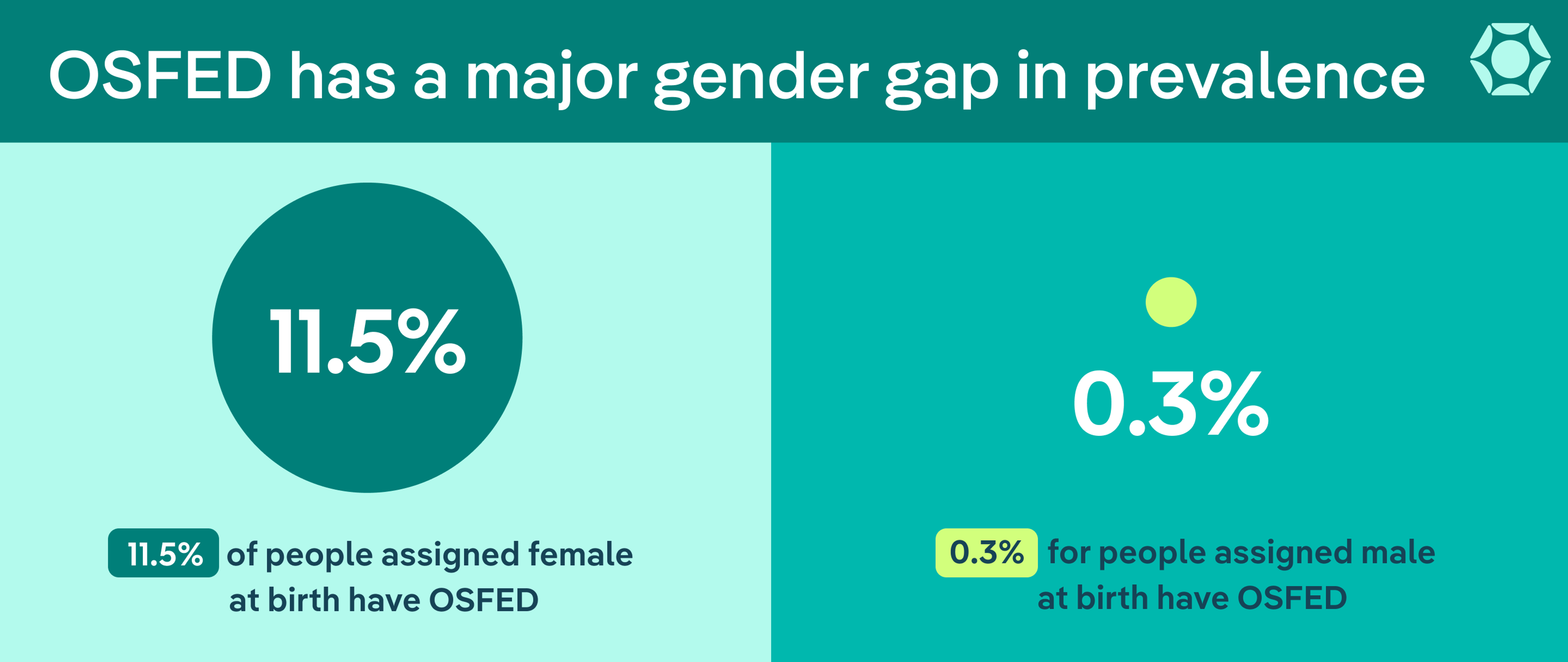
OSFED statistics: Despite not being as well-known, OSFED is a common eating disorder, with an estimated prevalence of up to 11.5% for people assigned female at birth and 0.3% for those assigned male.
OSFED vs EDNOS
Eating disorders are mental health conditions outlined in the Diagnostic and Statistical Manual of Mental Disorders 5th Edition (DSM-5), the guide that clinicians use to help diagnose eating disorders based on specific criteria.
Previous editions of the DSM used the term EDNOS, starting in 1987. But the DSM-5, which was published in 2013, officially retired the term in favor of using OSFED. The goal was to provide more information about the condition and to aid clinicians in diagnosing it so that patients like me could get appropriate care and treatment.
OSFED isn’t a perfect umbrella term, but the DSM-5’s updated language also includes more detail about the eating disorders that fall under it, helping to home in on what might be going on for patients.
What types of eating disorders fall under OSFED?
Several specific diagnoses fall under the OSFED umbrella. A brief look at these helps showcase why the term is needed to help more patients, especially those of us whose situation doesn’t fit neatly into a different category.
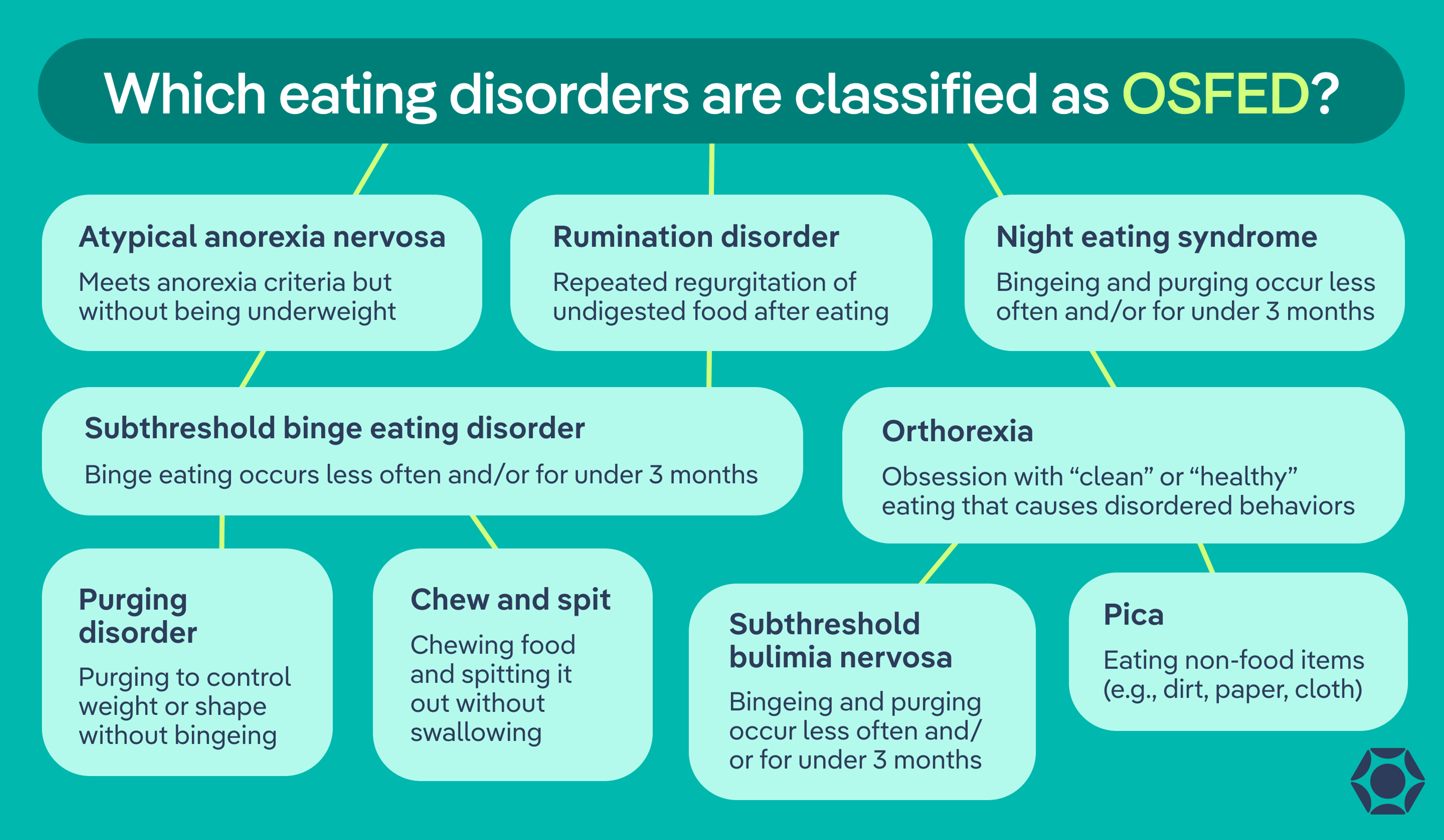
- Atypical anorexia nervosa (AAN): This condition shares all the criteria for anorexia nervosa except that people with AAN are not considered underweight.
- Subthreshold binge eating disorder: This condition shares all the criteria for binge eating disorder except that the binge episodes occur at a lower frequency and/or for less than three months.
- Subthreshold bulimia nervosa: This eating disorder shares all the criteria for bulimia nervosa except that the binging and purging behaviors occur at a lower frequency and/or for less than three months.
- Purging disorder: People with this condition engage in purging behavior to control weight or alter body shape but they do not binge. Purging might include vomiting, misusing laxatives, or exercising excessively.
- Night eating syndrome (NES): This condition involves eating at night, whether after waking up or binge eating after dinner. Clinicians diagnose it when behavior doesn’t align with binge eating disorder or another condition.
- Other types of OSFED: The five conditions noted above are common forms of OSFED, but they do not make up an exhaustive list. Other conditions that could also fit under the umbrella of OSFED, but don’t always, include the following:
- Rumination disorder: This disorder involves a pattern of regurgitating undigested food from the stomach to then be spit out, rechewed, or reswallowed, usually within 15 minutes of eating it.
- Chew and spit disorder: This disorder involves a repeated pattern of chewing and then spitting out food before swallowing. This is also not a formal DSM diagnosis, but symptoms could be diagnosed under the umbrella of OSFED.
- Pica: This condition involves eating things that aren’t food, such as dirt, cloth, paper, and more.
- Orthorexia: This condition, though not considered a formal eating disorder, involves obsessing over “healthy eating” or “clean eating,” leading to disordered behaviors surrounding food and exercise. The focus might include eliminating entire categories of food, such as dairy, carbohydrates, gluten, or “white” foods without a medical reason (e.g., a diagnosed allergy, sensitivity, or intolerance).
Note, though, that Pica and Rumination disorders are each their own distinctive diagnosis, not OSFED. But sometimes those with symptoms not meeting the full criteria could be diagnosed with OSFED. Keep in mind also that you can have OSFED without fitting neatly into any of these subcategories.
| Condition | Described in DSM-5 | Common behaviors | Misconceptions |
| Atypical anorexia nervosa (AAN) | Meets all DSM-5 criteria for anorexia nervosa except that body weight is not below normal despite significant restriction and weight loss | Severe food restriction, intense fear of weight gain, distorted body image, rigid food rules, compulsive exercise | Often dismissed based on weight, leading people to assume it is less serious or not an eating disorder |
| Subthreshold binge eating disorder | All features of binge eating disorder are present, but binge episodes occur less frequently or for less than three months | Episodes of eating large amounts of food with loss of control, eating rapidly, eating when not hungry, guilt or distress afterward | Commonly mistaken for “normal overeating” or “lack of self-control” rather than a clinically significant disorder |
| Subthreshold bulimia nervosa | Meets criteria for bulimia nervosa except that bingeing behaviors occur at lower frequency or for less than 3 months | Binge eating followed by purging behaviors (vomiting, laxatives, excessive exercise), strong body dissatisfaction | Often minimized because behaviors are “not frequent enough,” despite mental and physical health risk |
| Purging disorder | Recurrent purging behaviors to influence weight or shape without binge eating | Self-induced vomiting, laxative or diuretic misuse, excessive exercise | Frequently misunderstood as bulimia, or overlooked entirely because binge eating is absent |
| Night eating syndrome (NES) | Recurrent episodes of night eating (after awakening or excessive intake post- dinner) that do not meet criteria for BED or another disorder | Skipping breakfast, strong urge to eat at night, sleep disturbances, distress related to night eating | Often confused with late-night snacking or assumed to be a sleep issue rather than an eating disorder |
| Rumination disorder | Repeated regurgitation of food shortly after eating, which may be rechewed, reswallowed, or spit out | Regurgitating undigested food within ~15 minutes of eating, usually without nausea or disgust | Commonly mistaken for vomiting, acid reflux, or intentional purging |
| Chew and spit disorder (not a formal DSM diagnosis) | Repeated chewing of food followed by spitting it out before swallowing | Chewing food for taste, spitting it out to avoid calorie intake | Often seen as a “harmless habit” rather than dangerous eating disorder behavior |
| Pica | Persistent eating of non-food substances | Eating paper, cloth, chalk, dirt, or similar items | Frequently misunderstood as curiosity or cultural behavior instead of a diagnosable disorder |
| Orthorexia | Not a formal DSM-5 diagnosis, but recognized as a fixation on healthy or “clean” eating | Eliminating entire food groups, rigid food rules, anxiety around “unhealthy” foods, compulsive exercise | Often praised as discipline or wellness rather than recognized as disordered eating |
What are common signs and symptoms of OSFED?
Pinpointing signs and symptoms of OSFED on your own can be difficult, since you or a loved one might have symptoms associated with multiple eating disorders. For example, if I were to take my own symptoms and treat the table in the section above like a personal bingo card, I would blot the squares for atypical anorexia, purging disorder, and orthorexia.
In this section, we’ve categorized the behavioral, psychological, and physical signs and symptoms associated with OSFED across the board. If you or a loved one is experiencing any of these signs, talking to a knowledgeable clinician is a good idea. These symptoms can dramatically affect quality of life and physical and mental health.
Behavioral signs
- Avoiding certain food categories (e.g., dairy, gluten, carbs, etc., without a diagnosed medical reason).
- Binge eating or feeling as if you have no control around food
- Chewing food and spitting it out before swallowing
- Compulsive or rigid exercise routines or rules
- Developing rituals around food (e.g., cutting food into tiny piece or eating slowly)
- Eating large quantities of food after dinner or in the middle of the night
- Eating non-food items (e.g., paper or chalk)
- Eating secretively or having difficulty eating in social situations
- Following rigid food rules
- Obsessive focus on eating “clean”
- Purging behaviors (laxative misuse, self-induced vomiting, exercising excessively)
- Regurgitating food soon after eating
- Restricting food intake
- Skipping meals or eating small portions
Psychological signs
- Anxiety when foods you deem “safe” aren’t available
- Denial or minimization of serious behaviors
- Developing rituals around food (e.g., cutting food into tiny piece or eating slowly)
- Difficulty recognizing hunger or fullness cues
- Distorted body image
- Distress related to eating patterns at night
- Feeling out of control around food
- Intense fear of gaining weight or changing body shape
- Perfectionism or rigid thinking
- Preoccupation with food, meal timing, calories, or ingredients
- Strong feelings of anxiety, shame, or guilt regarding food or activity level
- Tying self-worth to eating habits, exercise habits, or body size or shape
Physical signs
- Brain fog
- Changes in appetite
- Dental or throat irritation, brought on by vomiting or regurgitating
- Dizziness or lightheadedness from inadequate nutrition
- Feeling cold frequently
- Gastrointestinal issues (e.g., bloating, constipation, or abdominal pain)
- Significant weight gain
- Significant weight loss
- Nutritional deficiencies
What are the health risks of OSFED?
“The health risks of OSFED can be just as serious as those of any other eating disorder,” Levine says. “Because OSFED covers many patterns, the risks vary, but the potential harm should never be underestimated.”
OSFED can increase the risk for mental health conditions, including anxiety, depression, obsessive-compulsive disorder, substance use disorder, and more. And the list of physical health risks is extensive.
Physical health risks of OSFED
- Dental issues
- Difficulty concentrating/brain fog
- Digestive issues (e.g., constipation, diarrhea, stomach or esophageal damage)
- Electrolyte imbalances
- Fatigue
- Heart problems
- Infertility
- Muscle loss
- Nutrient deficiencies
- Obesity
- Organ failure
- Osteoporosis
- Slowed growth in adolescents
- Type 2 diabetes
- And more
Is the term OSFED helpful?
“The term OSFED can actually be very helpful when it’s understood for what it is: an inclusive diagnosis,” explains Levine. “It exists to recognize people whose eating disorder symptoms are serious and disruptive but don’t fit neatly into those clinical boxes.”
She adds, “Rather than excluding those individuals, OSFED ensures they are seen, taken seriously, and able to access appropriate treatment and support. When explained clearly to patients and their supports, I think it can be reassuring, communicating that you don’t have to meet a rigid checklist for your experience to be valid or worthy of care.”
For me, landing on the term EDNOS was super helpful. And now with the newer term OSFED and its more robust definition, I have an even better understanding of what I was going through when I was younger. I didn’t fit super clearly into a category, but I needed help, and I’m so glad I got it. I also am now able to recognize if an old pattern or behavior crops up, see it for what it is, and take action for care.
“One important thing to highlight,” Levine adds, “is that you don’t need a ‘perfect’ diagnosis to deserve help. OSFED is common, treatable, and valid. Recovery isn’t about fitting into a label. It is about feeling better, getting support, and rebuilding a healthier relationship with food and yourself.”
What does OSFED treatment look like?
Appropriate OSFED treatment is tailored to you or your loved one with the condition. It often looks different, depending on your unique set of behaviors, thought patterns, symptoms, and any co-occurring conditions. Plus, multiple forms of treatment may be necessary.
However, Levine notes several common treatment approaches:
- Cognitive behavioral therapy for eating disorders (CBT-E)
- Family-based treatment (FBT)
- Nutrition support through working with a registered dietitian
“At Equip,” Levine says, “we do this as a team and make sure patients have access to a holistic approach that meets them where they are at and ensures they have access to the care they both want and need. Treatment focuses on both physical health and the underlying thoughts, emotions, and coping patterns connected to food and body image.”
The bottom line
OSFED is a serious mental health condition. It’s just as serious as other more well-known eating disorders, such as anorexia nervosa, bulimia nervosa, and binge eating disorder and requires personalized treatment for you or a loved one.
But I want to leave you with a huge dose of hope: recovery is possible with a knowledgeable and passionate care team. I wish Equip had existed when I was in my 20s, but I’m happy to report that I’m fully recovered. Triggers sometimes crop up, but I now have the understanding and the tools to navigate them and cope. I’m ever grateful to my friend who connected me to the right therapist and to that therapist for helping me heal.
FAQ
What does OSFED mean?
OSFED stands for other specified feeding and eating disorder. It is an umbrella term for diagnosing and giving name to a clinically significant feeding or eating disorder that does not match criteria for other feeding or eating disorder diagnoses.
What is EDNOS now called?
Eating disorder not otherwise specified (EDNOS) is now called other specified feeding and eating disorder (OSFED).
Can you have OSFED and ARFID?
Avoidant/restrictive food intake disorder (ARFID) is a distinct eating disorder, so if you or a loved one meet diagnostic criteria, the diagnosis is ARFID. However, sometimes people meet some but not all criteria for ARFID and may also meet some but not all the criteria for other feeding or eating disorders. In these cases, other specified feeding and eating disorder (OSFED) becomes the diagnosis.
Can you recover from OSFED?
Yes, you can recover from other specified feeding and eating disorder (OSFED) with the help of a knowledgeable and compassionate care team.
Is OSFED serious?
Yes, other specified feeding and eating disorder (OSFED) is just as serious as more well-known eating disorders, such as anorexia nervosa, bulimia nervosa, binge eating disorder, and more.
Aouad, Phillip, et al. “Chew and Spit (CHSP): A Systematic Review.” Journal of Eating Disorders, vol. 4, no. 1, Aug. 2016, p. 23.
Friederich, Hans-Christoph, et al. “Treatment Outcome in People with Subthreshold Compared with Full-Syndrome Binge Eating Disorder.” Obesity (Silver Spring, Md.), vol. 15, no. 2, Feb. 2007, pp. 283–87.
Johnson, Sarah N., et al. “An Empirical Evaluation of the Diagnostic Threshold between Full-Threshold and Sub-Threshold Bulimia Nervosa.” Eating Behaviors, vol. 42, July 2021, p. 101540.
Kusnik, Alexander, and Sarosh Vaqar. “Rumination Disorder.” StatPearls, StatPearls Publishing, 2025.
Nella, Ethan, and Jennifer Couturier. “Time to Recognise the Risks to Patients after an Eating Disorder Diagnosis.” BMJ Medicine, vol. 4, no. 1, Nov. 2025, p. e002261.
“Other Specified Feeding or Eating Disorders (OSFED) | NEDA.” National Eating Disorders Association, Accessed 6 Jan. 2026.
Salman, Ethar J., and Rian Kabir. “Night Eating Syndrome.” StatPearls, StatPearls Publishing, 2025.
Silén, Yasmina, and Anna Keski-Rahkonen. “Worldwide Prevalence of DSM-5 Eating Disorders among Young People.” Current Opinion in Psychiatry, vol. 35, no. 6, Nov. 2022, pp. 362–71.







